1- Pain on fire
As awful as it may feel, pain is meant to help us by warning us that a part of our
body
is injured and needs attention. Usually, pain signals work just fine. They fire when there is damage to a part of the body and turn off when the damage is resolved. Sometimes, however, these signals can fire inappropriately, warning us of danger when there isn’t any (or long after the danger has passed).
 If a person experiences pain for three months or more, it’s called chronic pain. There are numerous types of chronic pain disorders, each of which is characterized by the part of the body that’s in pain.
If a person experiences pain for three months or more, it’s called chronic pain. There are numerous types of chronic pain disorders, each of which is characterized by the part of the body that’s in pain.
6- Anxiety and depression
The cause of fibromyalgia is not known, but studies show that people with the disorder have a heightened sensitivity to pain, so they feel pain when others do not. Brain imaging studies and other
research
have uncovered evidence of altered signaling in neural pathways that transmit and receive pain in people with fibromyalgia. These changes may also contribute to the fatigue, sleep disturbances, and cognitive problems that many people with the disorder experience.
 Fibromyalgia tends to run in families, so genetic factors are likely to contribute to the disorder, but little is known for sure about the specific genes involved.
Fibromyalgia tends to run in families, so genetic factors are likely to contribute to the disorder, but little is known for sure about the specific genes involved.
Psychiatric problems seem to contribute considerably to the development of fibromyalgia. The prevalence of psychiatric conditions among patients affected by fibromyalgia is higher than among subjects complaining of other rheumatic diseases [ 3 ]. The most common disorders associated are anxiety, somatization, dysthymia, panic disorders, posttraumatic stress, and overall depression [ 106 – 110 ]. Depression is more frequently associated with fibromyalgia than with other musculoskeletal diseases [ 111 ] and the dysfunction of the 5-ht system might play a role [ 112 ]. Depression worsens fibromyalgic symptoms and vice versa, and antidepressants represent a cornerstone of fibromyalgia therapy [ 113 – 115 ].
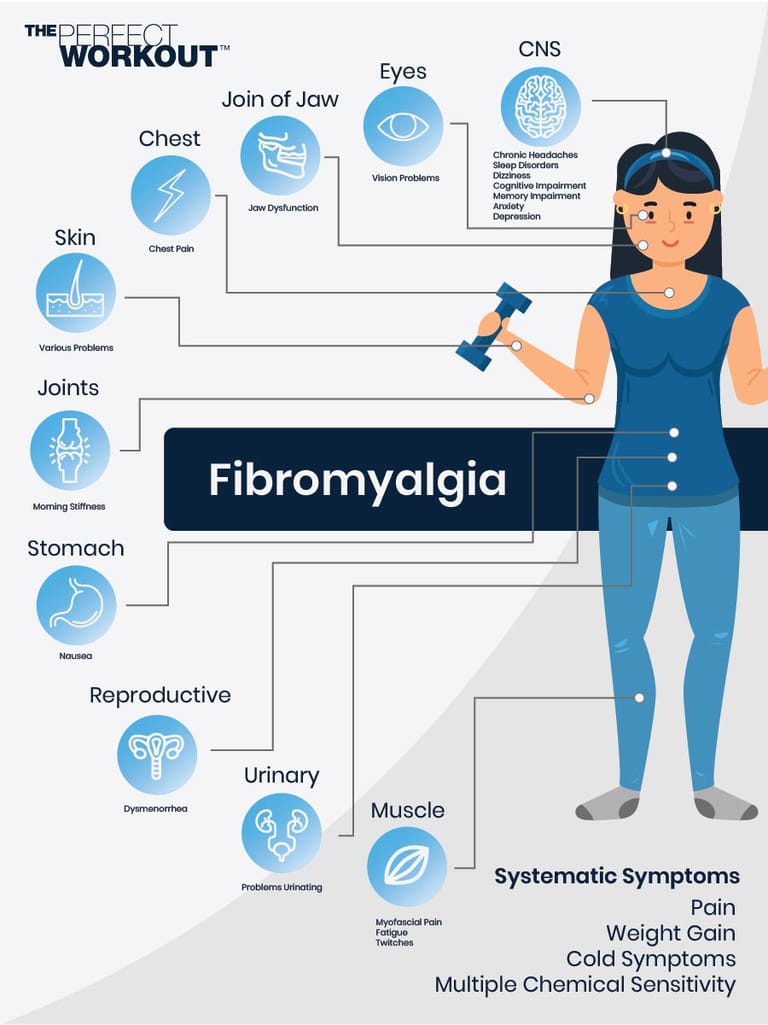
Symptoms of fibromyalgia include chronic widespread pain in the muscles, joints, back or neck. Other symptoms can include chronic fatigue, disturbed sleep, difficulty concentrating or remembering things (also known as “fibro fog”), depression/anxiety, headaches and gastrointestinal problems. Unfortunately, a lot of these fibromyalgia symptoms can mimic those of many other diseases, and this can make diagnosis challenging. For example, some people with fibromyalgia are misdiagnosed as having depression, rheumatoid arthritis or lupus, as these diseases share some of the same symptoms. Hypothyroidism, sleep apnea, degenerative spinal diseases, hiv and cancer also share many of the same symptoms of fibromyalgia. Because the symptoms can suggest multiple diseases, doctors need to rule the other diseases out first as they look for an explanation.
The symptoms of fibromyalgia can vary from mild to severe. The most common symptoms are: increased sensitivity to pain due to a decreased pain threshold increased responsiveness to sensory stimuli such as heat, cold, light and smell extreme fatigue (tiredness) numbness or tingling in the arms and legs anxiety and depression. Not everyone will experience all of these symptoms. Each person with fibromyalgia will have their own unique set of symptoms. The symptoms of fibromyalgia can vary from day to day. Symptoms may disappear for extended periods of time, perhaps even years.
Signs and Symptoms of Fibromyalgia
Basics of fibromyalgia "fibromyalgia" is a name used to describe generalized muscular pain and fatigue. Fibromyalgia is a set of signs and symptoms that occur together (a sign is what the physician finds on examination; a symptom is what a person reports to the doctor). Although fibromyalgia may feel like a joint disease, it is not a true form of arthritis and does not cause deformities of the joints. Prognosis fibromyalgia is not damaging to the body, but it may be a chronic condition. A carefully planned treatment program is essential. With proper management and a positive attitude, most people with fibromyalgia improve and are able to deal with their condition.
Everything you need to know about fibromyalgia
1. Pain and soreness the most general symptom of fibromyalgia is chronic pain all over the body parts. It is considered a primary symptom that leads patients to diagnose themselves and pursue treatment. It weakens your body for the long term. This pain can be stated in different ways. It can be dull, loud, sore, or painful. It can be felt in any of the body parts like in muscles, ligaments, joints tendons, etc. For some patients the pain is bearable and consistent on the other hand for some patients pain is unbearable and increasing day by day. 2. Fatigue fatigue and lingering tiredness are other symptoms that show in patients suffering from fibromyalgia.
Arnold lm, choy e, clauw dj, et al. Fibromyalgia and chronic pain syndromes: a white paper detailing current challenges in the field. Clin j pain. 2016;32(9):737–746. Doi:10. 1097/ajp. 0000000000000354 sluka ka, clauw dj. Neurobiology of fibromyalgia and chronic widespread pain. Neuroscience. 2016;338:114–129. Doi:10. 1016/j. Neuroscience. 2016. 06. 006 eken a, gökçay d, yılmaz c, baskak b, baltacı a, kara m. Association of fine motor loss and allodynia in fibromyalgia: an fnirs study. J mot behav. 2018;50(6):664-676. Doi:10. 1080/00222895. 2017. 1400947 vincent a, whipple mo, rhudy lm. Fibromyalgia flares: a qualitative analysis. Pain med. 2016;17(3):463-468. Doi:10. 1111/pme. 12676 leite ma, orsini m, de freitas mr, et al.
Fibromyalgia (fm) is a medical condition defined by the presence of chronic widespread pain , fatigue , waking unrefreshed , cognitive symptoms , lower abdominal pain or cramps , and depression. Other symptoms include insomnia and a general hypersensitivity. The cause of fibromyalgia is unknown, but is believed to involve a combination of genetic and environmental factors. Environmental factors may include psychological stress , trauma , and certain infections. The pain appears to result from processes in the central nervous system and the condition is referred to as a "central sensitization syndrome".
The burden of living with fibromyalgia is higher than with other rheumatic disorders and higher than with most other chronic illnesses. 1 , 9 , 10 , 28 as the medical management of fibromyalgia is often only partially successful, 2 health professionals need to give patients sustained support to become expert, active self-managers. This is the most important of all interventions to enable successful living with this debilitating multidimensional disorder. However, cognitive dysfunction related to the fibromyalgia, which is often not recognised by treating professionals, can make this process challenging. Growing evidence suggests self-management skills training is best delivered within a supportive small group setting where education, coping skills training, and cognitive behavioural approaches can be explored.
Main signs and symptoms
Stiffness and pain frequently begin gradually and diffusely and have an achy quality. Pain is widespread and may worsen with fatigue, muscle strain, or overuse. Patients typically have a variety of somatic symptoms. Fatigue is common, as are cognitive disturbances such as difficulty concentrating and a general feeling of mental cloudiness. Many patients also have symptoms of irritable bowel syndrome symptoms and signs irritable bowel syndrome is characterized by recurrent abdominal discomfort or pain with at least two of the following characteristics: relation to defecation, association with a change in frequency. Read more , interstitial cystitis symptoms and signs interstitial cystitis is noninfectious bladder inflammation that causes pain (suprapubic, pelvic, and abdominal), urinary frequency, and urgency with incontinence.
Comments
Post a Comment